Global healthcare systems reveal a mosaic of approaches to organizing, funding, and delivering care, inviting us to explore how policy choices, cultural expectations, and economic constraints shape outcomes across regions, populations, and time, and to consider the long arc from historical models to contemporary reforms, a perspective that illuminates both progress and persistent gaps. By examining healthcare models worldwide and universal health coverage case studies, we learn what tends to work, what fails, and why context matters for reform, while recognizing that success often depends on political will, governance capacity, resource allocation, the incentives embedded in funding mechanisms, and the ability to translate policy into everyday practice. This isn’t about declaring a single best model but about examining comparative health systems, noting strengths, trade-offs, and the conditions under which reforms succeed, including how primary care networks, hospital capacity, pharmaceutical policy, and data systems interact to deliver timely, affordable, and high-quality care, while guarding against unintended disparities. The insights from diverse settings highlight how health system reform around the world can improve access, quality, and resilience without sacrificing sustainability, using lessons from tax-funded systems, social health insurance, mixed public-private arrangements, and variations in private provision to illustrate the spectrum and guide localized adaptation. Together, these perspectives empower policymakers, providers, and communities to translate lessons into practical, patient-centered improvements that are adaptable, scalable, and sensitive to local values, capacity, and cultural expectations while maintaining a clear eye on equity and long-term financial protection.
From a parallel vocabulary, the topic can be framed using terms like international health systems, care delivery architectures worldwide, and policy-driven reform pathways to reveal how different jurisdictions balance access, quality, and cost without prescribing a single template. These terms align with latent semantic indexing principles by associating related concepts such as financing structures, governance arrangements, and health outcomes, encouraging a richer map of how care is organized and financed across settings. The broader view acknowledges that universal coverage is a spectrum shaped by politics, culture, and resources, and it invites cross-border learning without losing sight of local realities. By examining outcomes and experiences through diverse frames, decision-makers can extract transferable lessons that inform reform strategies and support steady improvements in efficiency, equity, and resilience.
Global healthcare systems: insights from universal access, financing, and governance
Global healthcare systems demonstrate a wide variety of financing mechanisms, from general tax revenue to mandatory insurance schemes. This panorama mirrors the diversity of healthcare models worldwide, where each approach balances financial protection with provider incentives. Across universal health coverage case studies, the common thread is protecting households from catastrophic costs while ensuring access to essential services. Governance choices—centralized planning, shared decision-making, or mixed models—shape how quickly reforms can be implemented and how performance is measured, highlighting the ongoing relevance of comparative health systems in shaping policy.
However, context matters: culture, economics, and administrative capacity influence which combination of financing and governance delivers results. The key takeaway from the global healthcare systems literature is not a universal blueprint but a menu of options that can be adapted. Effective reform emphasizes sustainable financing, strong primary care, and transparent data systems, all of which appear across universal health coverage case studies and in discussions of health system reform around the world. By analyzing comparative health systems, policymakers can identify what works locally while borrowing lessons from abroad.
Translating lessons into reform: practical pathways from comparative health systems to health system reform around the world
Translating these lessons into concrete reforms requires a practical toolkit grounded in evidence from comparative health systems. A blended financing model—combining public funding with strategic private participation—can spread risk and expand capacity while protecting vulnerable populations. Investing in primary care and prevention reduces the need for costly specialist services and strengthens resilience in the face of aging populations and new health threats. Across healthcare models worldwide, such strategies are repeatedly highlighted in policy discussions and universal health coverage case studies as levers for affordability and quality.
Beyond financing, robust data infrastructure, patient-centered care, and governance reforms that empower local decision-making are essential. When jurisdictions align incentives, ensure accountability, and involve communities in priority setting, health system reform around the world becomes more credible and sustainable. The literature on comparative health systems emphasizes that reforms succeed when they are context-aware yet informed by shared principles—equity, access, quality, and financial protection—found in universal health coverage case studies and global evaluations of healthcare models worldwide.
Frequently Asked Questions
How can global healthcare systems inform universal health coverage case studies and health system reform around the world?
Global healthcare systems show that financing, access, and governance must be aligned to achieve universal health coverage and sustainable reform. Through universal health coverage case studies, policymakers examine how tax-funded, social health insurance, or mixed financing influence coverage, costs, and quality of care. By studying comparative health systems, nations identify shared principles—financial protection, equity, and strong primary care—while adapting policies to local context and capacity. There is no one-size-fits-all model; the most successful reforms combine sustainable financing with transparent governance and data-driven improvement.
What factors shape outcomes when comparing healthcare models worldwide within global healthcare systems?
Key factors include the design of financing (public, private, or mixed), level of access, and governance structures that set priorities and accountability. Other crucial elements are the strength of primary care, preventive services, and robust data systems that enable performance monitoring. Equity and patient experience matter too, ensuring services are timely and culturally competent. By analyzing comparative health systems, policymakers can translate lessons from global healthcare systems into targeted reforms that improve coverage, affordability, and quality.
| Theme | Core Idea | Key Points |
|---|---|---|
| Foundations: Financing, Access, and Governance | Three interdependent pillars | Financing determines who pays and how much; Access governs who can obtain care when needed; Governance shapes priority setting, accountability, and performance. When these pillars are aligned, patients receive timely, affordable care; misalignment leads to gaps, longer waits, and worse outcomes. There is no one-size-fits-all formula; sustainable financing that protects against out‑of‑pocket costs supports universal health coverage. |
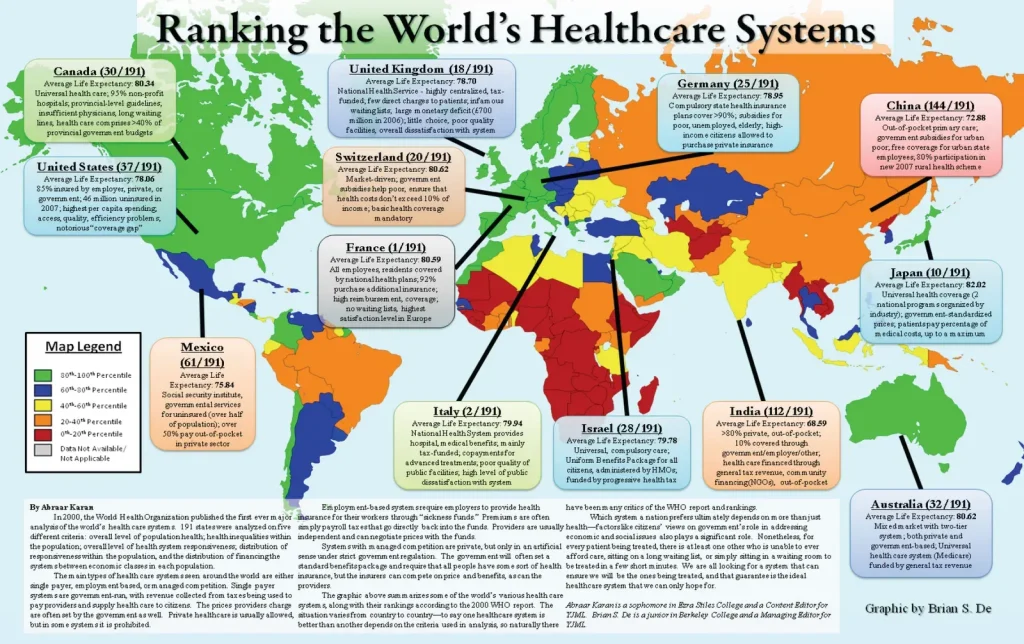
| Global Case Studies | Diverse national models and trade-offs | UK: universal access funded by taxation; Canada: universal essential services with provincial delivery leading to some access and wait variations; Germany: social health insurance with broad coverage and pluralistic providers; Nordic states: generous benefits and strong primary care with higher taxes; Singapore: hybrid model with regulated competition and targeted subsidies; United States: market-oriented system with high expenditure and less universal coverage. |
| Measuring Success | Outcomes, Equity, and Patient Experience | Outcomes include life expectancy, disease burden, and preventable hospitalizations; Equity asks whether all groups receive timely care regardless of income, geography, or ethnicity; systems with strong primary care tend to better preventive care and smoother transitions, while heavy reliance on emergency care can raise costs and fragmentation. |
| Translating Lessons to Reform | Practical Pathways for Improvement | Sustainable financing—combine public funding with strategic private participation where feasible; strengthen primary care and prevention to curb expensive interventions; invest in robust data systems for continuous quality improvement and accountability; advance patient-centered care with cultural competence and language access; implement governance reforms that empower local decision‑making within national standards; pursue a portfolio of policies to steadily improve coverage, affordability, and quality without sacrificing sustainability. |
Summary
Global healthcare systems are best understood as evolving frameworks that balance financing, access, and governance to deliver universal, high-quality care while shielding people from financial hardship. By comparing how different nations organize funding, access, and oversight, we can distill universal principles and adapt them to local contexts. The ultimate goal remains clear: universal access to essential services, strong quality of care, and robust financial protection against catastrophic costs. As demographics shift and technology reshapes care, the study of Global healthcare systems provides a durable lens for policymakers, practitioners, and citizens seeking sustainable improvements that prioritize people’s health and well-being.